The thyroid gland, which is shaped like a butterfly and located in the neck, plays a crucial role in controlling the body’s metabolism. Its hormones have an impact on every cell, tissue, and organ in the body. But how are these hormones released and regulated? Let’s explore this comprehensive guide to better understand the intricate dance of thyroid hormone regulation.
Thyroid hormones are vital for the overall functioning of the body. Their activity is carefully regulated at different stages to maintain a balance that promotes optimal health. The main point of regulation occurs during the synthesis of these hormones by the thyroid gland. In this section, we’ll delve into the fundamental processes that govern the release of thyroid hormones.
Thyroid hormones don’t just magically appear. Their release is the result of a series of coordinated steps, starting from the brain and culminating in the thyroid gland. This process ensures that the body receives the appropriate amount of hormones it requires.
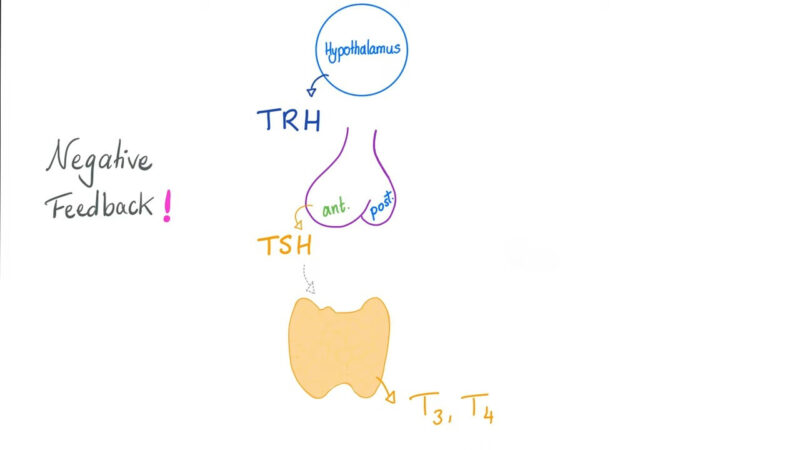
Basic Circuitry
Regulating the release of thyroid hormones is a complex dance involving various organs and hormones. This system oversees the fundamental coordination between the hypothalamus and pituitary gland, making sure the thyroid gland generates and releases the appropriate quantity of hormones.
1. Hypothalamic Step
In our brains, there’s this tiny region called the hypothalamus, nestled at the base. It’s like the conductor of an orchestra, releasing a hormone called thyroid-releasing hormone (TRH) to communicate with the anterior pituitary.
This hormone tells the pituitary gland to get to work, producing and releasing important hormones. TRH is a multitasker and also has a hand in the controlled release of prolactin, another essential hormone.
Thyrotropin-releasing hormone (TRH) is a hypothalamic hypophysiotropic neuropeptide that was named for its ability to stimulate the release of thyroid-stimulating hormone in mammals. It later became apparent that it exerts a number of species-dependent hypophysiotropic activities that regulate other pituitary hormones. – Haruhiko Kanasaki
2. Pituitary Step
When TRH sends its signal, the anterior pituitary gland springs into action, busy synthesizing and releasing Thyroid Stimulating Hormone (TSH). This hormone has a direct impact on the thyroid gland, nudging it to produce and release thyroid hormones.
3. Thyroid Step
When the thyroid gland gets stimulated by TSH, it does something pretty interesting. Instead of directly releasing the active hormones, it mainly releases T4, which doesn’t have much hormonal effect on its own. So, where does the real deal hormone actually come from?
4. Tissue Step
This is where the magic unfolds. The thyroid gland does its thing by releasing T4, which is later transformed by target tissues.
These tissues have an enzyme called Iodinase, which works its wonders by converting T4 into either T3 or rT3. T3 is the active form that packs a punch with important hormonal effects, while rT3 doesn’t do much.
This conversion that happens in the peripheral target tissues can be seen as the last step in the regulation of thyroid hormones.
Actions of TSH
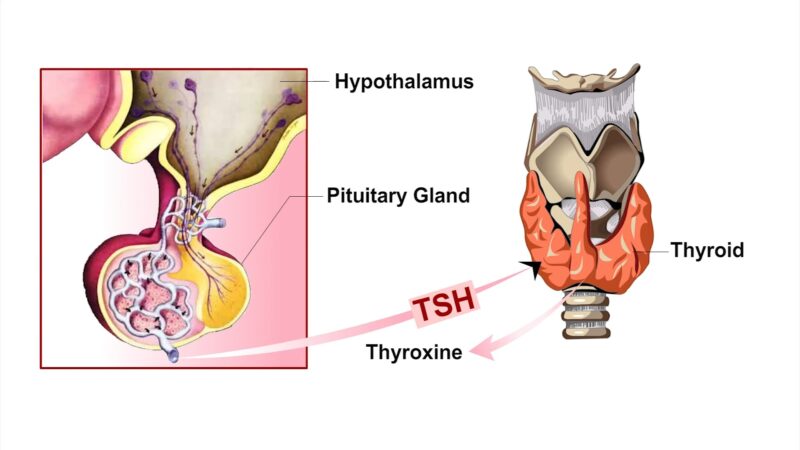
TSH is more than just a messenger hormone. It has a significant impact on the thyroid gland, affecting both the immediate and long-term synthesis of thyroid hormones.
When it comes to regulating thyroid function, TSH is a force to be reckoned with. It not only stimulates the rapid release of thyroid hormones but also boosts the gland’s ability to produce these hormones for an extended duration. How does it accomplish this remarkable feat?
Immediate Effects
When it comes to Thyroid Hormone Synthesis, TSH plays a key role in activating each and every step. One of the most important actions it takes is triggering the endocytosis of thyroglobulin that has been processed by peroxidase. This ultimately leads to the rapid release of thyroid hormones.
Long-term Effects
TSH plays a crucial role in supporting the thyroid gland. It not only causes the thyroid follicular epithelial cells to grow bigger (hypertrophy) but also increases their number (hyperplasia). As a result, the thyroid gland becomes visibly enlarged.
However, when there’s excessive stimulation, as seen in conditions like Graves Disease, it can cause thyrotoxicosis and result in an abnormal and excessive enlargement of the thyroid gland.
As per MountSinai, Graves Disease is an autoimmune disorder that leads to an overactive thyroid gland (hyperthyroidism).
Regulation of Thyroid Hormone Release
Thyroid hormones play a crucial role in our bodies, and their release is carefully controlled. The main control point for this process is the release of TSH from the anterior pituitary gland. However, we wonder: what exactly influences this release, and how is a harmonious equilibrium maintained?
Maintaining the release of thyroid hormones is a complex interplay of various factors. It involves a delicate dance between stimulation and inhibition. The primary stimulator in this dance is TRH, which originates from the hypothalamus.
On the other hand, the main inhibitor is the free and unbound T3 hormone. This balance ensures the proper functioning of our thyroid system.
Stimulation by TRH
Hypothalamic TRH is the primary factor that prompts the anterior pituitary to release TSH. This hormone then acts on the thyroid gland, stimulating it to release its hormones.
Negative Feedback by T3
Free, unbound T3 has a negative feedback effect on the anterior pituitary. It reduces the release of TSH, ensuring that the levels of circulating thyroid hormones remain stable in healthy individuals.
Regulation of Tissue Lodinase
As we’ve learned, the conversion of T4 to its active form, T3, is crucial for thyroid hormone activity. But how is this conversion regulated in target tissues?
The enzyme Iodinase in target tissues plays a pivotal role in determining the activity of thyroid hormones. It can convert T4 to either the active T3 or the inactive rT3.
Production of T3 and rT3
Usually, target tissues produce almost equal amounts of T3 and rT3. However, this ratio can change under specific conditions. For instance, during pregnancy, fasting, or certain diseases, a higher ratio of rT3 is produced. Conversely, in states of obesity, more T3 is produced.
Importance of Iodinase Regulation
Regulating Iodinase activity in target tissues is a crucial step in the thyroid hormone axis. It’s secondary, but still important, as it ensures that the body receives the appropriate amount of active thyroid hormone based on its specific requirements.
External Factors Influencing Thyroid Function
While the internal circuitry plays a pivotal role in thyroid hormone regulation, external factors can also significantly influence thyroid function. These factors can either enhance or inhibit the synthesis and release of thyroid hormones.
Dietary Influence:
Iodine plays a vital role in the production of thyroid hormones. If your diet doesn’t provide enough iodine, it can affect the synthesis of these hormones in a negative way. Conversely, consuming too much iodine can actually hinder the release of these hormones, which is referred to as the Wolff-Chaikoff effect.
The Wolff-Chaikoff effect is an effective means of rejecting the large quantities of iodide and therefore preventing the thyroid from synthesizing large quantities of thyroid hormones. – K Markou
Stress and Thyroid Function:
Chronic stress can influence the hypothalamic-pituitary-thyroid (HPT) axis. Elevated cortisol levels, a hallmark of chronic stress, can suppress TRH and TSH release, leading to reduced thyroid hormone production.
Thyroid Hormone Transport and Cellular Uptake
After they’re created, thyroid hormones don’t just stay put. They journey through the bloodstream, finding their way into specific cells where they unleash their powers. But how exactly do these hormones reach their intended targets, and what helps them get inside the cells?
Thyroid Hormone Binding Proteins:
In our bloodstream, we can find thyroid hormones tightly bound to proteins such as Thyroxine-binding globulin (TBG), Transthyretin, and Albumin. These proteins play a crucial role as carriers, ensuring that the hormones successfully reach their intended tissues.
Cellular Uptake Mechanism:
Thyroid hormones enter cells through specific transporters like MCT8 and OATP1C1. Once inside the cell, T4 can be converted to the active T3, exerting its metabolic effects.
Thyroid Hormone Receptors and Action
Thyroid hormones exert their effects by binding to specific receptors in target cells. These receptors are located in the cell nucleus and play a crucial role in mediating the actions of thyroid hormones.
Types of Thyroid Hormone Receptors:
There are two main types of thyroid hormone receptors: TRα and TRβ. These receptors have different tissue distributions, with TRα being predominant in the heart and TRβ in the liver and brain.
Mechanism of Action:
Upon binding to their receptors, thyroid hormones modulate gene expression. They can either activate or repress the transcription of specific genes, leading to changes in protein synthesis and, consequently, cellular activity.
Disorders of Thyroid Hormone Regulation
Just like any other bodily system, the thyroid hormone regulatory system can experience disruptions too. These disorders can cause a variety of symptoms and it’s important to diagnose and manage them promptly.
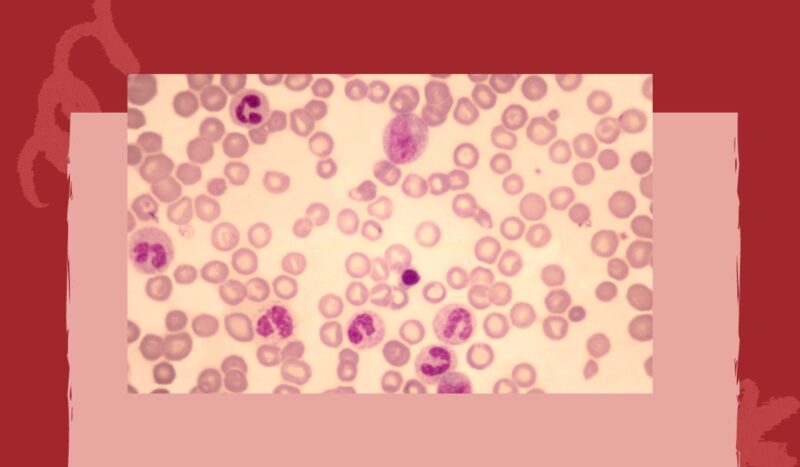
Hypothyroidism
This condition arises when there’s insufficient production of thyroid hormones. Causes can range from iodine deficiency to autoimmune disorders like Hashimoto’s thyroiditis. Symptoms include fatigue, weight gain, and cold intolerance.
According to Hopkinsmedicine, Thyroiditis refers to the inflammation of the thyroid gland. The most prevalent form of this condition is Hashimoto’s thyroiditis, which is classified as an autoimmune disorder. This happens when your body produces antibodies that mistakenly target and damage the cells within your thyroid.
Hyperthyroidism
In contrast, hyperthyroidism is characterized by excessive thyroid hormone production. Graves’ disease, an autoimmune disorder, is a common cause. Symptoms include weight loss, heat intolerance, and rapid heartbeat.