Starling Forces are essential principles that govern how water moves naturally between the tiny blood vessels called capillaries and the surrounding fluid known as interstitial fluid, which is the fluid that bathes our body’s cells. These forces play a vital role in maintaining the fluid balance in our body.
These forces determine the direction and speed at which water moves between the capillary and interstitial compartments. Put simply, Starling Forces decide whether water will move from the capillaries into the interstitial space, or the other way around, and how quickly this exchange will occur.
The balance between hydrostatic and oncotic pressures influences these forces. Hydrostatic pressure refers to the pressure exerted by the fluid on the walls of the blood vessels, which tends to push water out of the capillaries.
In contrast, oncotic pressure, primarily influenced by the concentration of proteins in the blood, pulls water back into the capillaries.
Key Variables
The direction of water exchange between the plasma and interstitial fluid across the capillary wall is largely determined by a combination of the relative hydrostatic and oncotic pressures of these two compartments. The rate of exchange is governed by the permeability of the capillary wall itself.
Hydrostatic Pressure Gradient
As per the University of Nottingham, Hydrostatic Pressure refers to the physical force of fluids against their enclosing barriers. Plasma within capillaries has a positive hydrostatic pressure, a remnant of the blood pressure generated by the heart.
Fluid within the interstitial place generally has a negative hydrostatic pressure, likely due to the action of lymphatic pumping.
Oncotic Pressure Gradient
According to Pujyitha Mandiga, Oncotic Pressure is all about the osmotic pressure created by protein-based solutes. You see, these special solutes can’t pass through the capillary barrier, so they end up being more concentrated in the plasma compared to the interstitial fluid.
That means the oncotic pressure in the plasma is higher than in the interstitial fluid, resulting in a gradient of oncotic pressure between these two compartments.
Vascular Permeability
Capillaries have a histological structure that influences how easily water can pass through them. Interestingly, this permeability can differ significantly between various capillary beds. Take the glomerular capillaries, for instance.
As Jeffrey H. Miner stated in his study, their fenestrated architecture allows them to be highly permeable to water.
On the other hand, the blood brain barrier has an incredibly tight architecture, resulting in extremely low water permeability.
It’s important to note that acute inflammation or specific types of capillary wall damage, like those experienced during burns, can actually increase water permeability in the microcirculation.
Formal Relationship
Starling Forces in Physiology
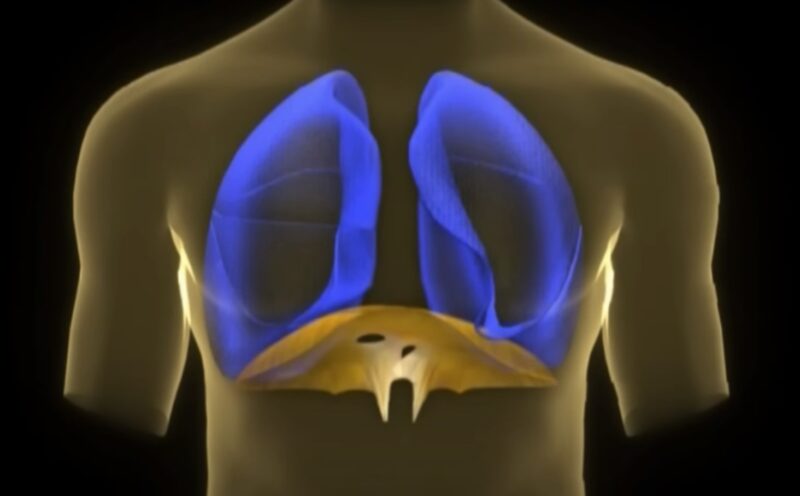
In most capillary beds, the way things work changes as blood flows through them. When blood reaches the arteriolar side of the microcirculation, it causes fluid to filter outwards due to starling forces. But as it reaches the venous side, starling forces cause the fluid to be absorbed back into the bloodstream.
Capillary beds help maintain a constant flow of blood through a process called autoregulation. – Lynne Eldridge, MD
These changes happen because the hydrostatic and oncotic pressures of the plasma fluid shift while blood travels through the microcirculation. It’s worth noting that the hydrostatic and oncotic pressures of the interstitial fluid mostly stay the same throughout this process.
Arterial Side
Capillary Hydrostatic Pressure (Pc) reaches its peak closest to the high-pressure arteries, while the interstitial hydrostatic pressure (Pi) remains consistently negative. On the arterial side of the microcirculation, the plasma oncotic pressure is relatively high, whereas the interstitial oncotic pressure is generally low or nonexistent.
As a result, the hydrostatic pressure gradient strongly promotes the outward filtration of water, while the oncotic pressure gradient encourages the inward resorption of water. Specifically, at the arterial side, the outward hydrostatic pressure gradient exceeds the inward oncotic pressure gradient, resulting in a net fluid filtration that occurs outwardly.
Of the factors determining fluid movement across the capillary wall, capillary hydrostatic pressure is likely to be the most variable, and is thus a major determinant of transcapillary fluid exchange. – I. R. Mahy, J. E. Tooke and A. C. Shore
Venous Side
As blood makes its way through the tiny blood vessels, specifically towards the venous side, the capillary hydrostatic pressure (Pc) decreases. This decrease is a result of the resistance encountered by the blood flow within the capillary.
Additionally, as the blood travels through the microcirculation, water is progressively filtered outwards, leading to an increased concentration of plasma proteins within the bloodstream. Consequently, the plasma oncotic pressure rises.
With the decrease in outward hydrostatic pressure gradient and the increase in inward oncotic pressure gradient, the overall effect is the resorption of fluid.
Net Filtration
In the tiny blood vessels of the body’s microcirculation, there is a balancing act between the filtration of fluid outwards on the arterial side and the filtration of fluid inwards on the venous side.
When we add up these filtration processes, we find that there is a very small overall outward flow of fluid from most capillary beds. If we calculate this outward flow across all the capillary beds in the body’s tissues, it appears that only a few milliliters of fluid are filtered outwards per minute.
Even though this outward filtration is minuscule, it is crucial to return the filtered fluid back into circulation to prevent long-term increases in the volume of fluid in the spaces between cells (interstitial fluid) and long-term decreases in the volume of circulating blood.
The lymphatic vessels, as discussed in the field of Lymphatic Physiology, play a key role in ultimately returning the filtered fluid to the circulation.
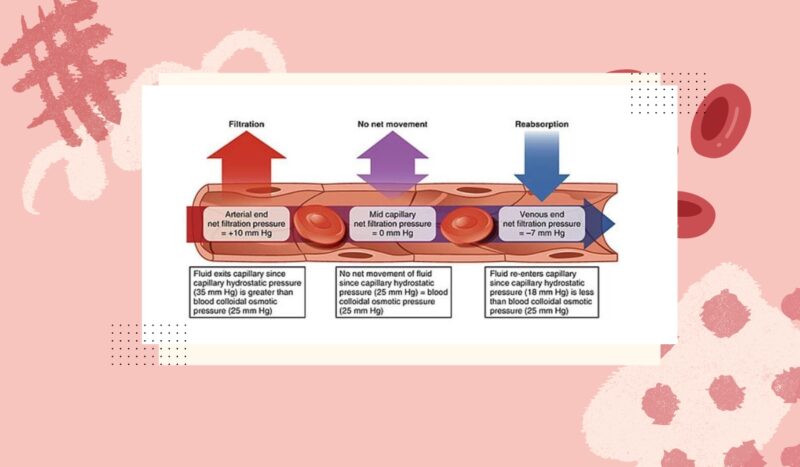
According to Aleksander S. Popel and Paul C. Johnson, the body’s microcirculation is composed of the tiniest blood vessels, including the capillary network with vessels ranging from 4-8 μm in inner diameter (i.d.), arterioles with a maximum diameter of approximately 100 μm (i.d.) in the arterial system, and venules, which are slightly larger vessels in the venous system. In essence, the microcirculation is a representation of the smallest blood vessels within the body.
Starling Forces in Pathology
A number of diverse pathological processes can derange the finely balanced fluid filtration of capillary beds by changing the key variables of the Starling Forces. In most cases this results in excessive water filtration out of the capillaries.
When this occurs locally it can result in localized edema whereas if it occurs globally throughout the body’s microcirculation, this can result in generalized edema. We provide a few examples below for didactic purposes.
1. Derangements of Vascular Permeability
Derangements of vascular permeability occur when the tight architecture of the capillaries is damaged. This can occur due to immune-mediated processes in acute inflammation or due to thermal damage in burns.
2. Derangements of Hydrostatic Pressure Gradient
When the hydrostatic pressure on the venous side of the microcirculation goes haywire, it’s often because there’s an abnormal increase in pressure.
This happens when blood isn’t effectively drained from the veins, leading to a buildup of blood and a subsequent rise in hydrostatic pressure on the venous side.
We call this condition congestion, and it can be caused by various factors such as venous thrombosis or right heart failure, just to name a couple of examples.
3. Derangements of Oncotic Pressure
Derangements of the oncotic pressure gradient usually occur due to reductions in plasma oncotic pressure from poor synthesis or excessive loss of plasma proteins, especially albumin. Reduced plasma oncotic pressure in turn reduces in the inward oncotic pressure gradient and thus allows for increased outward fluid filtration.
Reduced plasma protein synthesis, especially that of albumin, can occur in a variety of pathologies including protein-energy malnutrition, cirrhosis, and nephrotic syndrome.