The human body is truly incredible, filled with a multitude of intricate processes and pathways that work together to keep us alive. One of these pathways is heme degradation, a crucial mechanism that breaks down heme – the molecule that plays a central role in carrying oxygen.
In this article, we’ll discuss this fascinating process, exploring its different stages, its importance, and the chemistry that drives it.
A Quick Overview
Heme isn’t just an ordinary molecule; it’s the lifeblood of our red blood cells.
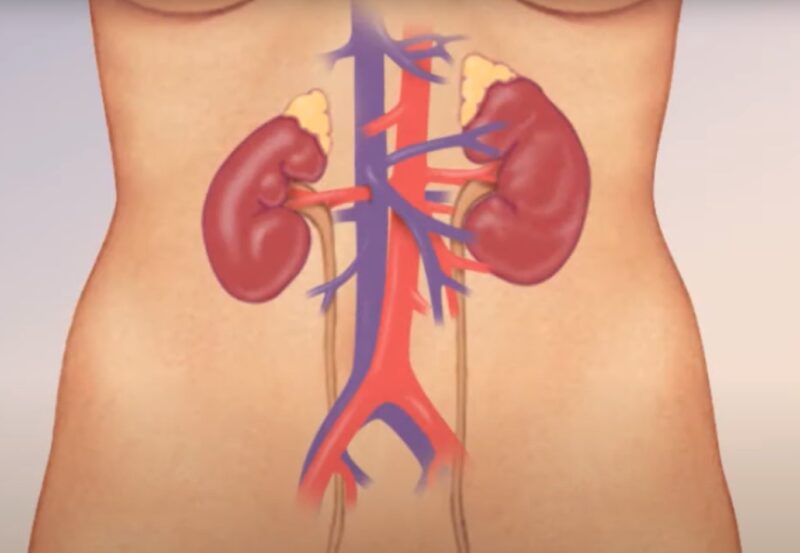
The process of breaking down and eliminating heme is like a beautifully orchestrated symphony, with approximately 80% coming from our aging red blood cells that have faithfully served us for around three months.
The remaining 20% comes from the young red blood cells in the bone marrow, which, for some unknown reason, don’t reach full maturity. A small, insignificant fraction also originates from other types of cells.
According to Marianna H. Antonelou, the aging process of red blood cells (RBCs) is regarded as a matter of unique scientific and clinical significance. It encompasses a complete set of unidirectional, time-dependent, yet not always linear molecular occurrences that ultimately result in the removal of the cell.
The Journey to Bilirubin
1. Bilirubin Production
When our old red blood cells reach the end of their journey, it’s mainly in the spleen and liver, where they bid their farewell, guided by the macrophages. Once these cells engulf them, something magical happens to the heme. It goes through a remarkable transformation, like a graceful dance choreographed by enzymes, with a quick pause known as “Biliverdin.”
This captivating process leads to the oxidation and opening of the heme ring, resulting in the birth of bilirubin. This newborn bilirubin, untouched by any chemical changes, is affectionately called “unconjugated” and swiftly released into the plasma by the caring macrophages.
As per Thomas R. L. Klei, Biliverdin is a compound that is both water-soluble and tetrapyrrolic, which is produced when heme is broken down. This breakdown process, facilitated by heme oxidase, results in the formation of biliverdin, iron, and carbon monoxide.
Subsequently, biliverdin undergoes a rapid breakdown into bilirubin, facilitated by the enzyme biliverdin reductase. An excessive accumulation of biliverdin and bilirubin, often caused by heightened hemolysis or liver damage that hampers glucuronidation, leads to the development of jaundice.
2. Homeward Bound: To the Liver
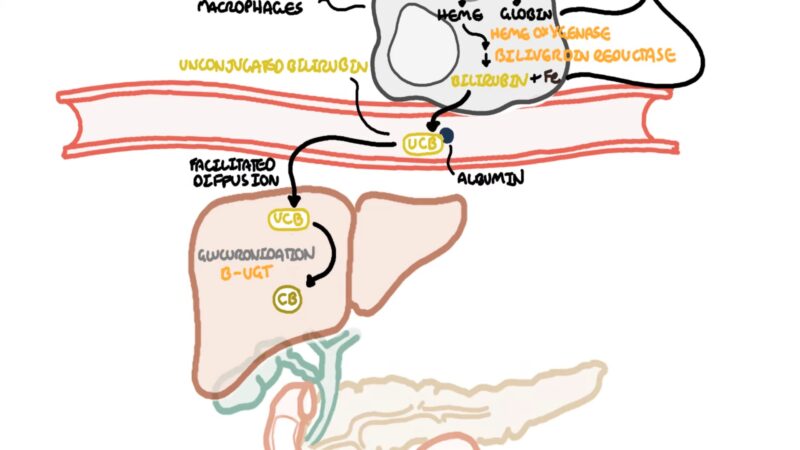
Unconjugated bilirubin isn’t the type that likes to mingle with water. But how does it manage to travel through the plasma? Well, it forms a close, though non-covalent, bond with albumin.
This strong connection guarantees that unconjugated bilirubin will never make its way into your urine. The adventure carries on until it arrives at the liver, where hepatocytes warmly greet the bilirubin and detach it from its albumin companion, ready to undergo further transformation.
3. The Conjugation
Inside these amazing liver cells, there’s a special enzyme called UGT1A1 that steals the spotlight. It works tirelessly, adding one or two glucuronic acid molecules to the bilirubin, transforming it into bilirubin mono- or di-glucuronide.
These newly formed substances, dressed up with glucuronic acid, are known as “Conjugated Bilirubin” and they’ve developed a real fondness for water.
The UGT1A1 gene belongs to a family of genes that provide instructions for making enzymes called UDP-glucuronosyltransferases. – MedlinePlus
4. Biliary Trip
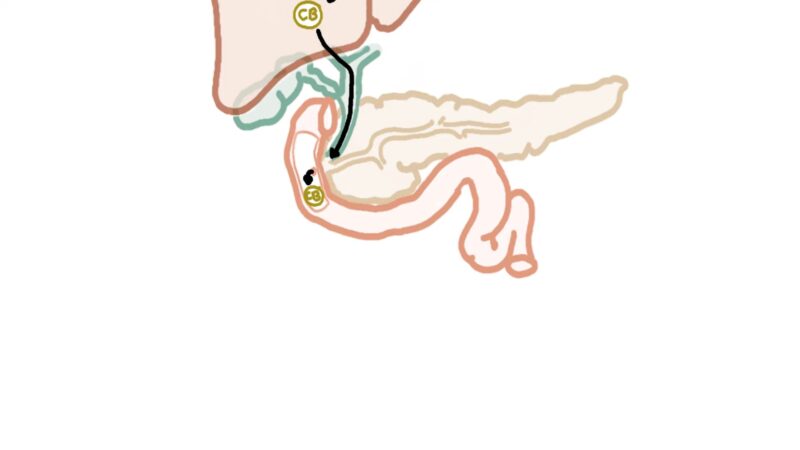
With its remarkable affinity for water, conjugated bilirubin is skillfully carried by hepatocytes into the bile canaliculi. It’s truly captivating to witness this process, as it demands both energy and meticulousness. Once bilirubin becomes a vital component of bile, it sets off on an adventurous journey along the biliary tree, ultimately reaching its destination in the duodenum.
From Bilirubin to Urobilinogens
When conjugated bilirubin reaches the busy community of GI bacterial flora in the gut, something interesting happens. These bacteria are quick to convert most of the bilirubin into a colorless substance called “Urobilinogen,” with a small portion turning into the brown pigment known as “Urobilin.”
But here’s where the story takes another turn. Around 90% of the urobilinogen decides to make its exit through the feces, leaving behind only a fraction that gets reabsorbed and sent back into the bloodstream.
However, this recycled urobilinogen doesn’t get far before it’s captured once again by hepatocytes and expelled through the bile. As a result, urobilin follows suit, contributing to the brown color of our feces. Yet, a tiny amount manages to be reabsorbed and makes its way to the kidneys, giving our urine a distinct yellowish hue.