Chronic Obstructive Pulmonary Disease (COPD) can be quite complex and is often surrounded by misconceptions. In this guide, we’ll discuss the disease, its causes, and symptoms. There’s a lot to cover, so let’s begin.
Overview
COPD is a chronic lung disease that affects people in the long run and can’t be reversed. It’s primarily caused by two conditions: emphysema and chronic bronchitis, which often occur together in the same patient.
Now, let’s discuss the shared factors that contribute to the development of COPD and explore how it presents clinically.
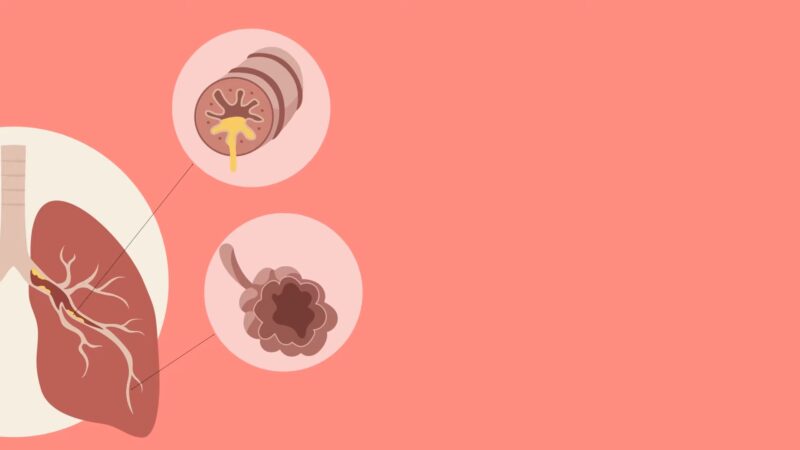
Emphysema
Emphysema is characterized by a reduction in the lung’s elastic recoil, leading to obstruction during expiration. This results in a decrease in the ability to force air out of the lungs.
As per Physio-pedia, individuals who have been diagnosed with emphysema might express that their primary symptoms include challenging or strenuous breathing, along with a decreased ability to exercise.
This is due to the loss of elastic recoil in the lungs, which results in permanent obstruction of the bronchi and overinflation of the lungs. Consequently, this leads to an increase in the volume of air beyond typical tidal breathing and functional residual capacity.
Chronic Bronchitis
When it comes to chronic bronchitis, the airways get narrower because of secretions from respiratory glands and goblet cells. It’s important to note that unlike asthma, the obstruction in COPD is irreversible and doesn’t show significant improvement even with bronchodilators.
Pathogenesis
Airflow Resistance
According to Anuj K. Agarwal’s research, COPD is mainly characterized by a persistent blockage in the airflow, making it harder for air to move through the airways.
This obstruction causes an increase in the resistance to airflow, which in turn results in a reduction of the Forced Expiratory Volume/Forced Vital Capacity ratio (FEV/FVC).
This decrease is a shared characteristic among various obstructive lung diseases.
Hyperinflation
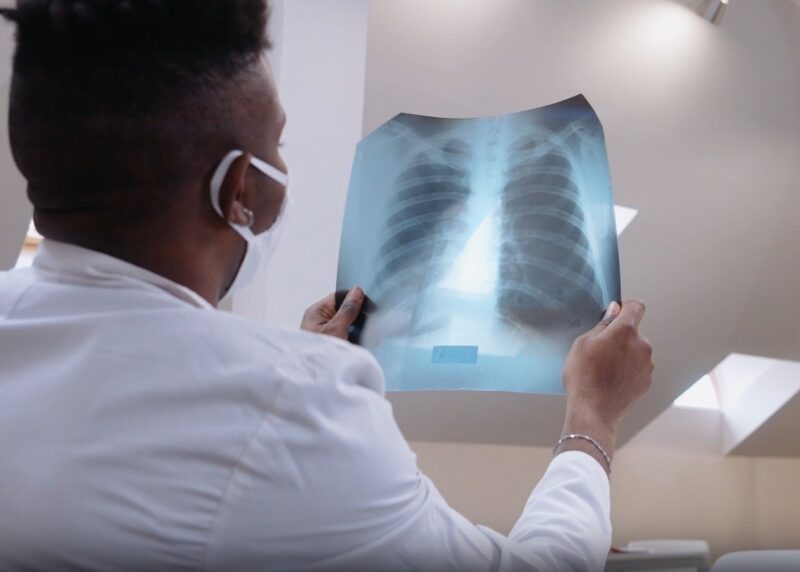
In late stages, the widespread obstruction can result in air trapping within the lung, known as hyperinflation. This is more severe in those with emphysema, leading to a “Barrel-shaped” chest and a flattening of the diaphragm on chest radiography.
Changes in Pulmonary Blood Flow
These patients may gradually develop pulmonary hypertension due to increased pulmonary vascular resistance. This can be exacerbated by increased blood viscosity from polycythemia, often observed in COPD patients due to chronic hypoxemia. Chronic pulmonary hypertension may eventually lead to right heart failure.
Changes in Gas Exchange
COPD results in profound ventilation-perfusion defects in the lung. Hypoxemia often develops with disease progression, and late-stage patients may begin to display hypercapnia due to hypoventilation.
Clinical Consequences
Pink Puffer
Characterized by progressive dyspnea, weight loss, and hyperinflation of the lungs. These patients often hyperventilate, maintaining adequate oxygenation, hence the term “pink puffer.”
Blue Bloater
These patients display progressive dyspnea and a long history of a worsening productive cough. They often have reduced respiratory drive, leading to hypoxemia and sometimes cyanosis. They tend to be more prone to right heart failure.