The Breathing Cycle is the amazing dance of pressures, volumes, and airflows that occur within our bodies as we take in oxygen and release carbon dioxide. It’s a rhythm we often overlook, yet it’s absolutely crucial for our very existence.
Picture your lungs as a pair of bellows, continuously expanding and contracting, providing your body with the vital oxygen it needs to operate and eliminating the waste product, carbon dioxide.
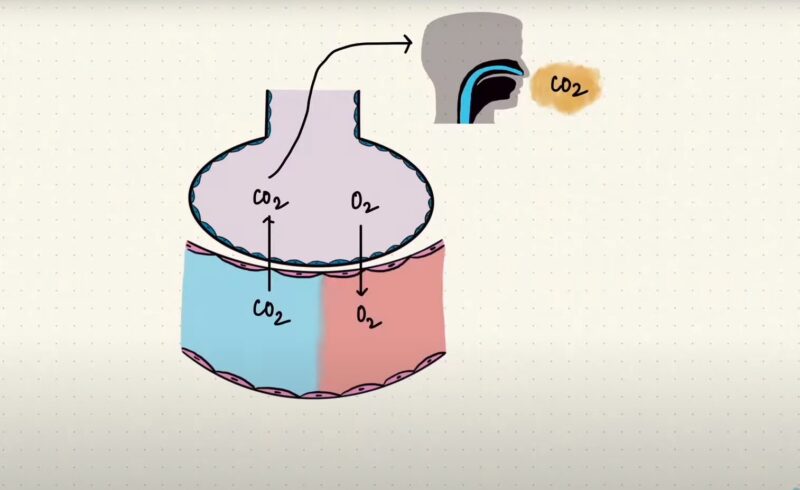
The key driving force behind this intricate process is the pressure difference between the air in your alveoli (those tiny air sacs in your lungs) and the space between your lungs and chest wall, known as the intrapleural space.
This pressure gradient is like the star performer, the conductor of an orchestra, orchestrating the expansion and contraction of your lungs in every single breath you take.
Now, you might wonder, why does this matter to you? Well, grasping the mechanics of your breathing cycle can help you truly appreciate the complexity behind this seemingly effortless process.
It can also guide you in various practices like mindful breathing or respiratory exercises, which offer a wide range of health benefits, from reducing stress to enhancing lung function.
Rest
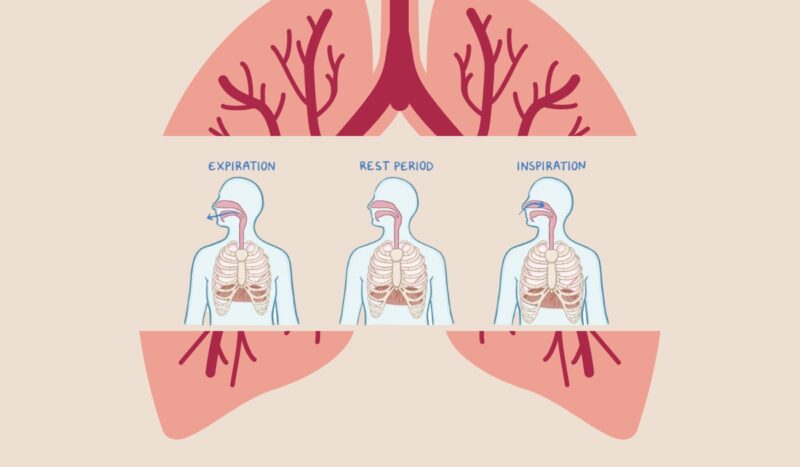
However, in a resting lung, the intrapleural pressure is typically around -5 cm H2O, which is five centimeters of water below the atmospheric pressure. This negative intrapleural pressure is a result of the opposing forces exerted by the lung and chest wall.
In Integrated Pulmonary Compliance, it’s explained that the lungs have a strong tendency to recoil at the FRC, while the chest wall has a tendency to expand outward. These opposing forces create a negative pressure within the intrapleural space, which keeps the lungs inflated while at rest.
If we were to eliminate this negative intrapleural pressure, for example, by raising it to match atmospheric pressure as can happen in a pneumothorax, the lungs would collapse due to their own recoiling force.
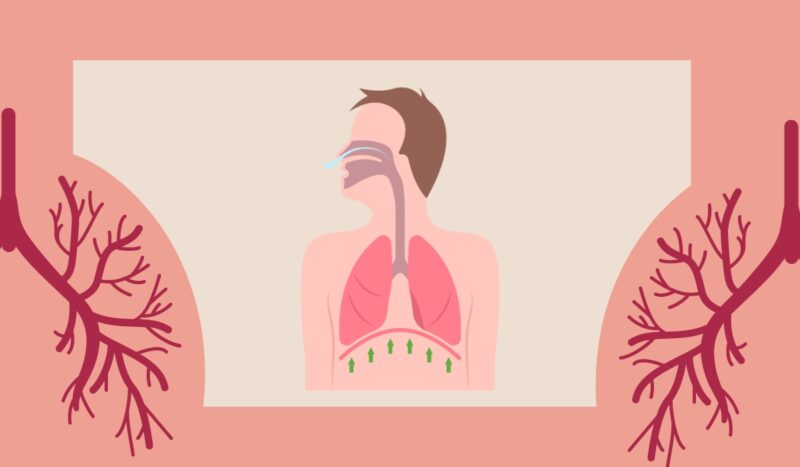
Inspiration
This influx of air indicates that the pressure in the tiny air sacs of the lungs, called alveoli, must be slightly lower than the atmospheric pressure.
As a result, air is drawn inwards. Simultaneously, the pressure within the space between the lungs and the chest wall, called the intrapleural pressure, also decreases, reaching a level around -7 or -8 cm H2O below atmospheric pressure. This drop in intrapleural pressure is a consequence of the lungs’ natural recoil, which generates a stronger pulling force as they expand.
Expiration
This outward movement of air indicates that the pressure within the alveoli, the tiny air sacs in the lungs, becomes slightly positive, surpassing atmospheric pressure.
As a result, air is propelled outwards. Throughout expiration, the lung’s elastic recoil diminishes as it contracts. Consequently, the pressure within the space between the lungs and the chest wall, known as the intrapleural pressure, reverts back to its original value of -5 cm H2O.
This restoration of pressure helps bring the lung volume back to its initial FRC.