The carotid bodies and aortic arch house these amazing peripheral chemoreceptors that play a crucial role in keeping our body in balance. They diligently keep an eye on the levels of oxygen (O2), carbon dioxide (CO2), and blood pH in our arteries, working tirelessly to maintain homeostasis.
These remarkable structures are an essential part of our respiratory control system, making sure that gas exchange and acid-base balance are carefully and precisely regulated. They truly embody the delicate harmony that our body strives to achieve.
Core Functions and Locations
Peripheral chemoreceptors, the carotid bodies situated at the bifurcation of the carotid arteries and the aortic bodies along the aortic arch, serve as the main hubs for sensing chemical changes in the bloodstream. Their clever positioning enables them to effectively monitor alterations in blood chemistry, playing a vital role in regulating respiration and metabolism.
Mechanisms of Action
Peripheral chemoreceptors play a crucial role in our body by detecting changes in the levels of oxygen, carbon dioxide, and blood pH. While scientists continue to investigate the intricate workings of these mechanisms, it is evident that these receptors are vital for responding to low oxygen levels in our arteries and fluctuations in blood acidity.
The carotid bodies are the major chemoreceptor sites for hypoxia and are very sensitive to changes in partial pressure of arterial oxygen (PaO2), arterial carbon dioxide (PaCO2), and H+. – Claude Gaultier & André Denjean
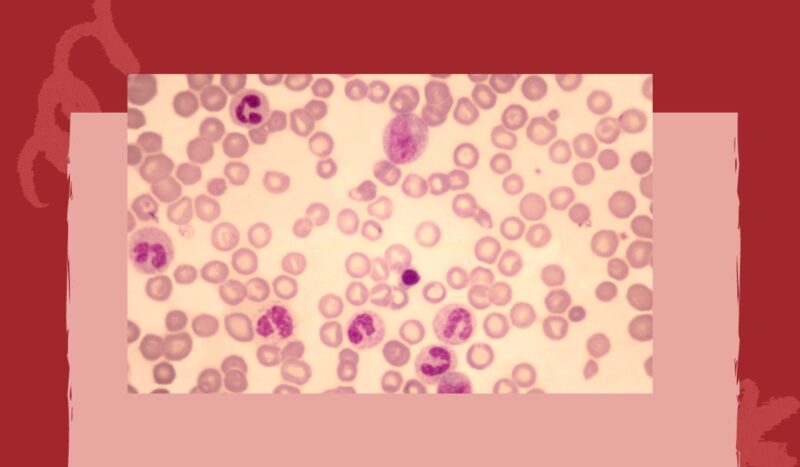
1. Oxygen Sensing
Peripheral chemoreceptors play a critical role in our body’s response to changes in arterial oxygen levels. When oxygen levels drop, these receptors become highly sensitive and send signals to the brain, prompting an increase in ventilation.
This important mechanism helps us adjust our oxygen intake when faced with hypoxemia, ensuring our body gets the necessary oxygen it needs to function properly.
2. Carbon Dioxide Detection
While peripheral chemoreceptors have the ability to sense variations in CO2 levels, their significance in responding to CO2 is not as crucial as that of central chemoreceptors found in the brain. The central chemoreceptors play a primary role in monitoring the concentration of arterial CO2.
3. pH Monitoring
Carotid body chemoreceptors possess an impressive capability to detect alterations in blood pH. These sensors are directly stimulated by shifts in acidity, regardless of the underlying reason, thus playing a vital role in the body’s ability to address acid-base imbalances.
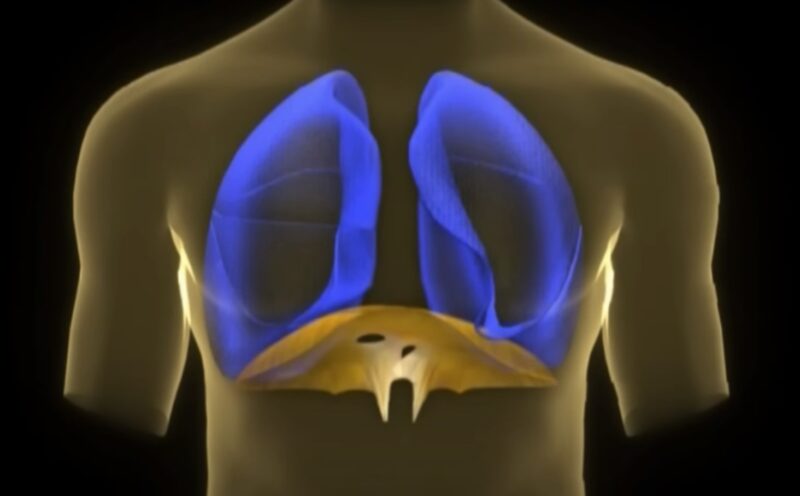
Impact on Respiratory Regulation
Peripheral chemoreceptors play a crucial role in regulating our breathing. They communicate with the respiratory centers in the brainstem, prompting adjustments in both the rate and depth of our breaths.
This feedback mechanism is essential for keeping our blood gas levels and pH in balance, ensuring that our body stays in a state of equilibrium.
Peripheral chemoreceptors monitor changes in arterial blood O2, and within seconds after the onset of hypoxia they trigger cardiorespiratory changes (i.e., increase in breathing and blood pressure), which are important for maintaining O2 homeostasis. – Nanduri R. Prabhakar
Cellular and Molecular Details
Receptor Mechanisms
- Peripheral chemoreceptors contain ion channels that respond to changes in O2, CO2, and pH. Oxygen-sensitive potassium channels, for example, play a key role in oxygen sensing, where a decrease in O2 levels leads to channel closure, cell depolarization, and neurotransmitter release.
- Hypoxia-inducible factors (HIFs) are critical in the cellular response to low oxygen, affecting chemoreceptor sensitivity and signaling to the respiratory centers in the brain.
Gene Expression
Genes such as PHD2 (prolyl hydroxylase domain-containing protein 2) and EGLN1 (encoding EGL-9 family hypoxia-inducible factor 1) are involved in oxygen sensing. Variations in these genes can influence peripheral chemoreceptor function and the individual’s respiratory physiology.